- Digitalization
Categories:
The healthcare sector is undergoing rapid digital transformation, and Cyber Physical Systems (CPS) are at the heart of this shift. These systems blend physical devices, real-time data, and computational intelligence into a single connected environment. In hospitals, clinics, and remote care facilities, CPS are enabling smarter decision making, improving patient outcomes, and supporting new ways of delivering care.
But with increasing reliance on connected systems comes the need for robust safety and cybersecurity frameworks. In a clinical environment, failure in either can lead to service disruption, harm to patients, and even loss of life. How are Cyber-Physical Systems transforming healthcare—and why is an integrated approach to security critical for their safe and successful adoption?
What are cyber-physical systems?
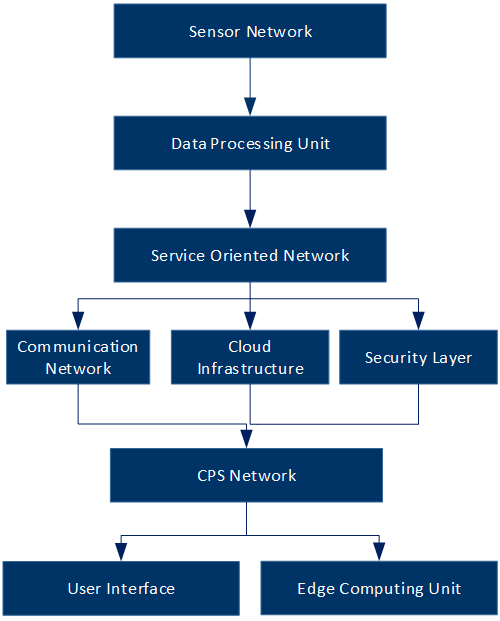
Cyber-Physical Systems (CPS) in healthcare are advanced integrated technologies that combine computational intelligence with physical processes to enhance medical care, diagnostics, and patient monitoring. These systems bring together sensors, medical devices, software, and secure connectivity to enable real-time interaction between hardware, software, and human physiology. CPS are used to monitor patients in real-time, automate hospital workflows, support remote consultations, and even drive AI-based diagnostics.
The value of CPS lies in their ability to gather and analyse data from medical devices and environments, then use that data to drive automated responses. For example, a wearable heart monitor can alert clinicians when a patient’s heart rate exceeds safe thresholds. On a larger scale, CPS can manage hospital infrastructure, ensure the readiness of critical equipment, and support large-scale telehealth and remote care services.
The healthcare impact
CPS are improving healthcare delivery across several dimensions. Clinically, they enable early detection of health issues, more accurate diagnosis, and tailored treatment. Operationally, they streamline processes, manage inventory, and reduce human error through automation.
Telemedicine is another area where CPS are proving critical. By connecting patients and providers through secure, real-time systems, CPS expand access to care and reduce geographic barriers. These capabilities are especially important in remote regions or during public health emergencies.
A growing number of healthcare providers are adopting intelligent platforms that combine cloud-based records, machine learning models, and real-time patient data. These platforms provide clinicians with decision support, increase transparency, and improve continuity of care across systems and facilities.
The healthcare impact: security is safety
While the benefits of CPS in healthcare are clear, they introduce complex risks. A system failure or cyberattack can have serious implications, including delays in critical care, data breaches, and equipment failure. As healthcare becomes more connected, ensuring security is essential.
Many healthcare systems were not originally designed with cybersecurity in mind. As a result, introducing CPS into existing infrastructure can create vulnerabilities if not properly managed. The ISA/IEC 62443 standard recognises that security must be embedded throughout the system lifecycle, from design to decommissioning.
For example, a connected infusion pump must be designed to deliver precise dosages while also preventing unauthorised remote access. If the system is not secured, an attacker could alter dosage settings or interrupt service delivery, creating a patient safety hazard.
Safety and cybersecurity should therefore be addressed as a single, unified concern. Protecting against unauthorised access, ensuring data integrity, and maintaining reliable operation all contribute to a safe system. The earlier these considerations are integrated, the more effective the overall result.
Lifecycle approach to CPS implementation
An integrated lifecycle approach is essential when deploying CPS in clinical environments. The system must be secure not only when installed but across its entire operational life. This includes regular updates, secure patching, performance monitoring, and end-of-life planning.
During the design phase, developers must identify potential cyber threats and define technical and organisational measures to mitigate them. Implementation involves secure configuration, limited user access, and test validation. Once deployed, systems must be monitored continuously, with all updates and changes handled through structured processes.
Decommissioning also requires care. Data must be safely removed, and system components must be retired without exposing sensitive information or disrupting ongoing operations. In a healthcare setting, failure to properly decommission equipment can pose compliance and liability risks.
Challenges in healthcare environments
Adopting CPS in healthcare is not without challenges. Many providers face legacy systems that lack compatibility with modern technologies. Bridging the gap between new CPS platforms and older infrastructure requires time, investment, and expertise.
Healthcare organisations also face increasing threats from cybercriminals. Hospitals have become prime targets for ransomware and data theft. Securing CPS devices—many of which have limited computing power—requires tailored security models that protect systems without degrading performance.
There is also a growing skills gap. Cyber-physical environments demand cross-disciplinary knowledge that spans IT/OT/IoT, operations, and clinical care. Without proper training, even well-designed systems can be misconfigured or underutilised.
Building a resilient CPS strategy
Achiving the full potential of CPS requires commitment of stakholders to a shared responsibility model. Asset owners must understand the risk profiles of their systems and ensure that safety and cybersecurity requirements are clearly defined. Product suppliers should provide secure, well-documented components. Integrators must configure systems correctly and ensure they are tested and validated before handover.
Healthcare organisations must also adopt a culture of continuous improvement. CPS environments evolve quickly, and threats are always changing. Regular assessments, audits, user training, and updates are all part of maintaining a secure and effective system.
Conclusion
Cyber-Physical Systems are driving a new era of healthcare that is smarter, faster, and more responsive. But with this innovation comes the need to consider security at every stage of the technology lifecycle. By adopting a lifecycle approach and aligning stakeholders across the healthcare ecosystem, we can build CPS that are not only effective but also resilient and trustworthy.
Whether managing hospital operations or monitoring patient health remotely, CPS offer a powerful way to improve outcomes. But their success depends on planning, collaboration, and a clear commitment to safety and cybersecurity.
- cybersecurity
Tags:
Soroush Tazerji
Director de servicios de seguridad de Tactix Sener Group
Soroush is Director of Security Services at Tactix Sener Group. He has extensive experience in large-scale railway projects in Australia, North America, and the Middle East. His expertise encompasses full project lifecycle management, including the design, implementation, testing, installation, commissioning, and operation of cybersecurity technology systems and operations. He has successfully provided cybersecurity solutions for various ICS/IACS systems, managed major cybersecurity improvement programs, and established cybersecurity operations and response units that are part of the Cybersecurity Operations Center (CSOC) for Critical Infrastructure. He also contributed to the development of international cybersecurity standards and automation and control systems.